Learn what DHA really is and why it is particularly important during pregnancy and throughout lactation
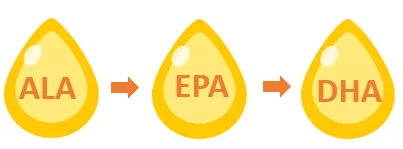
Docosahexaenoic acid (DHA) is a type of omega-3 fatty acids, alongside alpha-linolenic acid (ALA) and eicosapentaenoic acid (EPA).1,2 ALA is the parent fatty acid of the omega-3 family which is then converted to EPA, then on to DHA.1,3,4

DHA is one of the most biologically active omega-3 fatty acids.1 It is available in either active form (i.e. from diet rich in DHA e.g. fish or foods fortified with DHA) or formed through the conversion of ALA to EPA and DHA.4 Generally, the active form of DHA is better than the converted form because:
- Conversion of ALA to DHA is limited as most of the dietary ALA undergoes oxidation process (splitting of the long ALA chains into smaller fragments) in the cells and only a limited amount is converted to EPA and DHA4
- It has been shown that higher intake of ALA during pregnancy does not cause significant rise in DHA in the blood4,5
- In lactating mothers, ALA supplementation has no significant effect on the amount of DHA in breast milk5
Why is DHA important for pregnant/lactating women?
Adequate consumption of DHA in pregnant and lactating women is important as DHA is a critical component for the development of foetus’ cell membranes, particularly in the brain and retina.1,3,6 DHA supplementation is also associated with lower incidence of pre-term labour and delivery, lower risk of preeclampsia, increase in birth weight and reduction in postpartum depression incidences.7,8
During pregnancy, DHA requirements are increased over normal in order to support foetal growth; especially in the third trimester.1,8 This is due to increased maternal blood volume and enhanced placental and foetal DHA requirements.1,8,9 Pregnant women become depleted in DHA because the foetus utilises most of the DHA for its nervous system development and obtains about 67 mg/day of DHA from the mother.7,10 During lactation, the mother’s body transfers 70 to 80 mg of DHA daily through breast milk.10 The high requirement of DHA during pregnancy and lactation diminishes maternal DHA stores to below pre-pregnancy levels.10 Therefore, the Ministry of Health Malaysia suggests a DHA intake of 200 mg/day for pregnant mothers in order to meet the DHA demands.6
Why is DHA important for the foetus?
DHA is an essential building block for foetal brain development especially during the third trimester where the foetus’ brain undergoes ‘brain growth spurt’ or a period of rapid brain growth.3,10 Brain accumulation of DHA starts as early as the second half of gestation period.3,10
DHA is also a vital component and the major fatty acids of the eyes, comprising of 93% of all omega-3 fatty acids in the retina; suggesting its relevance in eye health and visual development.2,3,10

How to get DHA?

Listed below are the dietary sources of DHA:
· Fish (e.g. salmon, tuna, sardines, catfish, pollack,anchovies and herring)6,7,11
· Algae-derived marine oils11
· Eggs fortified with DHA12
Although fish are an important source of omega-3 fatty acids, it is advisable to limit the intake of certain types of fish (e.g. shark, tilefish, king mackerel and swordfish) as they may be potentially contaminated with methyl mercury, polychlorinated biphenyls or other toxins that can be dangerous to the foetus’ brain development.1,7,11 The United States Food and Drug Administration (FDA) and Environmental Protection Agency (EPA) recommend limiting fish consumption to 2 servings (340 g seafood) per week for pregnant women.1
What is the expert recommendation?
Listed below are some of the expert recommendations on DHA intake in pregnant and lactating women:
- The Ministry of Health Malaysia suggests a DHA intake of 200 mg/day for pregnant mothers6
- The Food and Agriculture Organization of the United Nations (FAO) recommends a minimum intake of 300 mg EPA+DHA per day of which at least 200 mg/day should be DHA for adult pregnant and lactating females7
- The Perinatal Lipid Nutrition Project (PeriLip) and The Early Nutrition Programming Project (EARNEST) in collaboration with several international scientific societies suggest an intake of at least 200 mg/day DHA for pregnant and breastfeeding women3
- The European Food Safety Authority (EFSA) recommends a 250 mg of EPA plus DHA intake daily (of which 100 to 200 mg should be DHA)8
Is there enough DHA in the diet?
In general, research has shown that the average daily intake of the omega-3 fatty acids (ALA + EPA + DHA) amongst the average Malaysian adults are far from desirable.6,13 Among pregnant Malaysian women, the mean intake of omega-3 was 0.24% kcal (Recommended Nutrient Intake; RNI = 0.45% kcal).13 Unsatisfactory omega-3 nutrition was also reported in lactating women i.e. 0.33% kcal as compared to the recommended 0.50% kcal.13

If mum eats fish, does she still need DHA supplementation?
The FDA recommends that women who are pregnant and breastfeeding consume 2 servings (340 g seafood) of fish per week.1,3,14 Nevertheless, even if you eat fish twice a week, you may not be getting the recommended levels of DHA. This is because the content of DHA varies among different fish species.15,16 In Malaysia, the most consumed fish are the Indian mackerel, anchovies and scad.6 However, these fish species contain low DHA levels as compared to salmon, herring, shad or bluefin tuna.15,16
Alternatively, DHA supplementation makes it easier to monitor your DHA intake to ensure that you are getting adequate DHA levels each day.17
How early to start on DHA supplementation?
As DHA is crucial throughout pregnancy and during lactation; especially for brain development, it is advisable that women take maternal nutritional supplements (e.g. DHA supplements) before or at the onset of pregnancy.2,10,18 This is to ensure that they have adequate nutrition stores so that pregnancy can start in a healthy state while reducing pregnancy complications.10,19
Article contributed by Dato’ Dr Siti Zaliha, Consultant Obstetrician & Gynaecologist
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only shall not be construed as medical advice or instruction. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website. No action or inaction should be taken based solely on the contents of this information; instead, readers should consult appropriate health professionals on any matter relating to their health and well-being. The information and opinions expressed here are believed to be accurate, based on the best judgement available to the authors, and readers who fail to consult with appropriate health authorities assume the risk of any injuries. In addition, the information and opinions expressed here do not necessarily reflect the views of Mead Johnson Nutrition (M) Sdn Bhd and its Affiliates. Mead Johnson Nutrition (M) Sdn Bhd and its Affiliates are not responsible for errors or omissions. Mead Johnson Nutrition (M) Sdn Bhd and its Affiliates do not recommend or endorse any specific tests, physicians, products, procedures, opinions or other information that may be mentioned on this website. Reliance on any information appearing on this website is solely at your own risk.
References:
- Coletta JM, Bell SJ, Roman AS. Reviews in Obstetrics and Gynecology
- Greenberg JA, Bell SJ, Ausdal WV. Reviews in Obstetrics and Gynecology. 2008;1(4):162-169.
- Koletzko B, Lien E, Agostoni C, et al. J Perinat Med. 2008;36(1):5-14.
- DHA/EPA/Omega-3 Institute. 2018. Available at http://www.dhaomega3.org/Overview/Metabolism-of-Omega-6-and-Omega-3-Fatt.... Accessed on 28 May 2018.
- Watson RR, Grimble G, Preedy VR, Zibadi S, editors. 2013; Volume 2. New York: Humana Press
- Ministry of Health Malaysia. Recommended Nutrient Intakes for Malaysia. 2017. Available at http://nutrition.moh.gov.my/wp-content/uploads/2017/05/FA-Buku-RNI.pdf. Accessed on 28 May 2018.
- American Pregnancy Association. Omega-3 fish oil and pregnancy. 2016. Available at http://americanpregnancy.org/pregnancy-health/omega-3-fish-oil/. Accessed on 28 May 2018.
- Hubinont C, Savoye T. Journal of Pregnancy and Reproduction 2017;1(1):1-7.
- Judge MP, Harel O, Lammi-Keefe CJ. Am J Clin Nutr. 2007;85(6):1572-1577.
- Morse NL. Nutrients 2012;4(7):799-840.
- World Health Organization. 2011. Available at http://www.who.int/elena/titles/bbc/fish_oil_pregnancy/en/. Accessed on 28 May 2018.
- Dietitians of Canada. 2013. Available at https://www.dietitians.ca. Accessed on 28 May 2018.
- Ng TKW, Nalliah S, Hamid A, Wong SR, Chee SL, Augustine CA. IeJSME. 2012;6(2):4-9.
- 2016. Available at https://www.babycenter.com/0_eating-fish-when-youre-breastfeeding-how-to.... Accessed on 31 May 2018.
- Wan Rosli WI, Rohana AJ, Gan SH, et al. International Food Research Journal 2012;19:815-821.
- S. Department of Agriculture and U.S. Department of Health and Human Services. 2010. 7th Edition, Washington, DC: U.S. Government Printing Office.
- 2017. Available at https://www.healthline.com/nutrition/how-much-omega-3. Accessed on 4 June 2018.
- American Pregnancy Association. 2018. Available at http://americanpregnancy.org/first-year-of-life/omega-3-supplements-baby/. Accessed on 29 May 2018.
- Carvajal JA. BioMed Research International. 2014;2014:526895.

